Predictive analytics can help to model potential virus spread. However, where monkeypox is concerned, the lack of familiarity[1][2] and the possibility that the virus may employ multiple routes of transmission[3] make even short-term modeling a challenge. In this article, Clarivate Consultant Thirumugam Muthuvel and Senior Science Editor Shyama Ghosh offer an inside view into the ‘how’ of predictive modeling and discuss valid models available from literature.
Confirmation of one case of monkeypox in a country is deemed an outbreak. Since May this year, the unpredicted emergence of monkeypox in areas without any epidemiological link to West and Central Africa suggests undetected transmission for some time[4][5][6]. A phylogenomic analysis of monkeypox virus genomes indicates that a novel clade may be responsible for the current outbreak, probably aided by the absence of smallpox immunity[7].
As of September 28, the World Health Organization (WHO) reported 66,471 laboratory confirmed cases, including 26 deaths. Infections occur mostly in men, in the 18-44 age group. The United States registered the highest number of cases (24,990), followed by Brazil, Spain, France, the United Kingdom and Germany. Infections are following a downward trend in Canada, as well as in some European countries, including Germany and the Netherlands.
Public awareness campaigns and media coverage are effective tools for educating the public on the monkeypox outbreak. These may help to reduce infections to very low levels; however, it is unclear whether these will be enough to eradicate the outbreaks altogether. This paper aims to understand the evolution of monkeypox by following the trend of new gene mutations expressed by the virus and interpreting the predictive data available from literature[8].
A rapidly-mutating, fast-traveling virus
The monkeypox virus is mutating fast – the current mutation rate is about twelve times higher than expected[16]. Speculating that the current 2022 strain is descending from the 2017 Nigeria outbreak, scientists anticipated around ten new mutations; instead, they found 50[9]. This is an indication that the virus is evolving rapidly through human-to-human transmission. It is mostly spreading through skin contact now and has a low R number (the rate at which the virus reproduces); however, it is mutating fast so a high level of genetic drift may be occurring[10]. Will this result in higher infectivity to humans? Also, will the mutations enable the virus to switch between hosts and reservoirs?
In contrast to COVID-19, monkeypox spreads through close contact, with little indication of airborne transmission. In the recent monkeypox outbreaks in Europe and North America, a significantly higher infectivity ratio was noted for men who have sex with men (MSM) compared to non-MSM cases[11]. This trend was also noted in the United Kingdom and suggests that the monkeypox virus has a low transmission potential outside high-frequency sexual contact groups[12].
Brand and colleagues from the University of Warwick estimated the risk of transmission per sexual contact at 31% (on May 1, 2022)[13]. Their research suggested that during the 2-week infectious period, populations with more than three sexual contacts may display higher R ratios than those with one.
Researchers modeling a 12-week look-ahead predicted that monkeypox cases would peak among the MSM population in the week beginning July. Thereafter, weekly case incidences would decline by September 2022 in this population (Figure 1).
Figure 1: U.K. Monkeypox forecast[13]

Source: Incidence and Prevalence Database from Clarivate
The epidemic trajectory (Figure 1) is evidence that the transmission potential per infected person (both MSMs and non-MSMs) has already decreased (~30%) since the outbreak began, because of public awareness that monkeypox is present/threatening and that its symptoms can be recognized.
Monkeypox infection outside of the MSM population is unlikely to be sustained based on current case data; public health messaging has already had a significant impact on reducing the risks of transmission by increasing awareness in both MSM and non-MSM populations. Rapid vaccine rollout has been prioritized to curtail transmission, resulting in a faster decline in cases.
Researchers at Georgia State University predicted that the monkeypox incidence would decline in the U.S., but it remains uncertain whether the disease can be eradicated (Figure 2)[14][15].
Figure 2: U.S. Monkeypox forecast (As on Sep 21, 2022)[14]
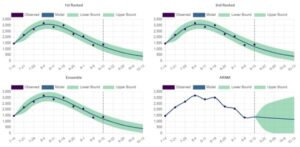
Source: Incidence and Prevalence Database from Clarivate
Public health measures can head off pandemics
Why do epidemics turn into pandemics? There are many causes and factors attached to this phenomenon. Despite all efforts, monkeypox infections have now spread across all six WHO regions. A precise prediction of future virus spread is difficult and may not be fully accurate when done. A modeling study reports on the potential growth of outbreaks in non-endemic countries. Scientists use modeling to predict outcomes under varying control measures (no intervention; contact tracing and surveillance; and ring vaccination). The model registers that public health responses (such as contact tracing and surveillance, isolating symptomatic cases, and ring vaccination) may significantly lower secondary cases by up to 86% and outbreak duration by up to 75%[10].
Dr. Tedros Ghebreyesus, Director General of the WHO, has warned that despite ongoing efforts to control COVID-19, up to 15,000 lives were lost due to the infection in one week at the end of August.
“We might be living with COVID-19 for the near future,” said Dr. Ghebreyesus, “but we do not have to live with monkeypox.”
While shining a light on the workings behind predictive modeling, it is prudent to discourage claims by data scientists about the million-wide monkeypox-infected cases predicted for September this year[16]. Further outbreaks can be avoided by tracking infections, effective public health measures and community involvement, all aimed at preventing transmission[17][18].
Clarivate predictive analytics tools are used by established and emerging global life sciences companies to anticipate barriers to innovation and speed new treatments to market, whether choosing clinical trial sites or prioritizing market entries. Data from the Clarivate Cortellis Incidence and Prevalence Database and Drug Discovery Intelligence™ Disease Briefings were used in this report. For more information on how Clarivate can help your company nurture innovation and protect its investments, contact us here.
This article was written by Shyama Ghosh, Senior Science Editor, and Thirumugam Muthuvel, Clarivate Consultant.
Literature references and web links visited:
[1]Center for Infectious Disease Research and Policy, 2022. Monkeypox Resource Center. [Online]
Available at: https://www.cidrap.umn.edu/monkeypox
[Accessed 20 October 2022].
[2]Carstens, A., 2022. Monkeypox: What We Know (and What We Don’t). The Scientist, 24 June.
[3]Soucheray, S., 2022. Monkeypox viral DNA detected in saliva, semen. [Online]
Available at: https://www.cidrap.umn.edu/news-perspective/2022/07/monkeypox-viral-dna-detected-saliva-semen
[Accessed 20 October 2022].
[4]The European Centre for Disease Prevention and Control and the World Health Organization, 2022. Joint ECDC-WHO Regional Office for Europe Monkeypox Surveillance Bulletin. [Online]
Available at: https://monkeypoxreport.ecdc.europa.eu/
[5]Anon., 2022. Global Health. [Online]
Available at: https://map.monkeypox.global.health/country
[Accessed 20 October 2022].
[6]Adesola Yinka-Ogunleye, O. A. M. D. D. O. A. M. Y. D. I. M. A. A. A. A. J. B. A. N. E. N. L. M. A. M., 2019. Outbreak of human monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. The Lancet Infectious Diseases, 19(8), pp. 872-879.
[7]Nicolas Luna, A. L. R. M. M. N. B. L. H. P. S. A. C. D. K. B.-A. A. P.-M. J. D. R., 2022. Phylogenomic analysis of the monkeypox virus (MPXV) 2022 outbreak: Emergence of a novel viral lineage?. Travel Medicine and Infectious Disease, Volume 49.
[8]Swift Centre, 2022. Monkeypox: the outlook for 2022. [Online]
Available at: https://www.swiftcentre.org/monkeypox-should-we-worry/
[Accessed 20 October 2022].
[9]Juta Medical Brief, 2022. Monkeypox mutating faster than expected — Lisbon scientists. [Online]
Available at: https://www.medicalbrief.co.za/monkeypox-mutating-faster-than-expected-lisbon-scientists/
[Accessed 6 July 2022].
[10]Soucheray, S., 2022. Virus causing monkeypox outbreak has mutated to spread easier. [Online]
Available at: https://www.cidrap.umn.edu/news-perspective/2022/06/virus-causing-monkeypox-outbreak-has-mutated-spread-easier
[Accessed 20 October 2022].
[11]Jesús Iñigo Martínez, E. G. M. S. J. B. F. M. M. A. N. J. J. S. D. N. G. M. E. C. D. A. N. F. M. A. G. A. M. H. N., 2022. Monkeypox outbreak predominately affecting men who have sex with men, Madrid, Spain, 26 April to 16 June 2022. Eurosurveillance, 27(27).
[12]Kupferschmidt, K., 2022. Why monkeypox is mostly hitting men who have sex with men. Science, pp. 1364-1365.
[13]Brand, S., 2022. Monkeypox UK. [Online]
Available at: https://github.com/SamuelBrand1/MonkeypoxUK
[Accessed 20 October 2022].
[14]Georgia State University School of Public Health Epidemic Forecasting Center, 2022. Forecasts of national monkeypox incidence in the United States. [Online]
Available at: https://publichealth.gsu.edu/research/monkeypox-forecasting-center/#091422
[Accessed 20 October 2022].
[15]Centers for Disease Control and Prevention, 2022. Monkeypox: 2022 U.S. Map & Case Count. [Online]
Available at: https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html
[Accessed 20 October 2022].
[16]Browne, E., 2022 . Monkeypox Models Suggest We Have No Idea What Outbreak Holds. Newsweek, 1 July.
[17]Rivers, C., 2022. Don’t lose sight of monkeypox containment. Nature, 31 August.
[18]Kozlov, M., 2022. Monkeypox in Africa: the science the world ignored. Nature, 23 June.





